TIGIT (/ˈtɪdʒɪt/ TIJ-it;[5] also called T cell immunoreceptor with Ig and ITIM domains) is an immune receptor present on some T cells and natural killer cells (NK).[6] It is also identified as WUCAM[7] and Vstm3.[8] TIGIT could bind to CD155 (PVR) on dendritic cells (DCs), macrophages, etc. with high affinity, and also to CD112 (PVRL2) with lower affinity.[6]
| TIGIT | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | TIGIT, VSIG9, VSTM3, WUCAM, T-cell immunoreceptor with Ig and ITIM domains, T cell immunoreceptor with Ig and ITIM domains | ||||||||||||||||||||||||||||||||||||||||||||||||||
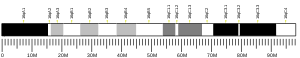
| External IDs | OMIM: 612859; MGI: 3642260; HomoloGene: 18358; GeneCards: TIGIT; OMA:TIGIT - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Numerous clinical trials on TIGIT-blockade in cancer have recently been initiated, predominantly combination treatments. The first interim results show promise for combined TIGIT and PD-L1 co-blockade in solid cancer patients.[9] Mechanistically, research has shown that TIGIT-Fc fusion protein could interact with PVR on dendritic cells and increase its IL-10 secretion level/decrease its IL-12 secretion level under LPS stimulation, and also inhibit T cell activation in vivo.[6]TIGIT's inhibition of NK cytotoxicity can be blocked by antibodies against its interaction with PVR and the activity is directed through its ITIM domain.[10]
Clinical significance
TIGIT regulates T-cell mediated immunity via the CD226/TIGIT-PVR pathway.[11]
HIV
During Human Immunodeficiency Virus (HIV) infection, TIGIT expressing CD8+ T cells have been shown to be expanded and associated with clinical markers of HIV disease progression in a diverse group of HIV infected individuals.[12] Elevated TIGIT levels remained sustained even among those with undetectable viral loads. A large fraction of HIV-specific CD8+ T cells simultaneously express both TIGIT and another negative checkpoint receptor, Programmed Death Protein 1 (PD-1) and retained several features of exhausted T cells.[12] Blocking these pathways with novel targeted monoclonal antibodies synergistically rejuvenated HIV-specific CD8+ T cell responses.[12] Further, the TIGIT pathway is active in the rhesus macaque non-human primate model, and mimics expression and function during Simian Immunodeficiency Virus (SIV) infection.[12] This pathway can potentially be targeted to enhance killing of HIV infected cells during "Shock and Kill" HIV curative approaches.[13]
Cancer
TIGIT and PD-1 has been shown to be over-expressed on tumor antigen-specific (TA-specific) CD8+ T cells and CD8+ tumor infiltrating lymphocytes (TILs) from individuals with melanoma.[14] Blockade of TIGIT and PD-1 led to increased cell proliferation, cytokine production, and degranulation of TA-specific CD8+ T cells and TIL CD8+ T cells.[14] It can be considered an immune checkpoint.[11] Co-blockade of TIGIT and PD-1 pathways elicits tumor rejection in preclinical murine models.[15] Numerous anti-TIGIT therapies have entered clinical development.
- Tiragolumab
Tiragolumab is the furthest progressed anti-TIGIT therapy in development. In non-small cell lung cancer (NSCLC) setting, the phase II CITYSCAPE clinical trial (NCT03563716) evaluated the combination of the anti-TIGIT antibody tiragolumab in combination with the anti-PD-L1 antibody atezolizumab in patients with newly-diagnosed non-small cell lung cancer whose tumors expressed PD-L1. After a median follow-up of 16.3 months, the combination of tiragolumab and atezolizumab reduced the risk of disease progression or death by 38% compared to atezolizumab monotherapy. In a subset of patients with high PD-L1 expression (at least 50% of tumor cells expressing PD-L1), the combination of tiragolumab with atezolizumab further reduced the risk of disease progression or death by 71% compared to atezolizumab monotherapy. Overall, patients who received the combination of atezolizumab and tiragolumab lived a median of 23.2 months, compared to 14.5 months with atezolizumab monotherapy.[16] Despite this initial success, there was concern that the benefit of PFS in the tiragolumab + atezolizumab arm was driven by the underperformance of atezolizumab in this trial.[17] Another concern was that there was no link between TIGIT expression and the efficacy of tiragolumab in the trial.[18]
The phase III, randomized, double-blinded SKYSCRAPER-01 trial, which evaluates the efficacy of the combination of tiragolumab and atezolizumab in NSCLC patients whose tumors have high PD-L1 expression, failed to show a significant PFS improvement in the combination arm compared with placebo + atezolizumab, although it showed "a numerical improvement" in both endpoints of PFS and overall survival (OS).[19] In August 2023, an internal PowerPoint presentation detailing OS data of the second analysis was mistakenly made public on the Internet and showed a numerical improvement in terms of OS [estimated overall survival after a median follow-up of 15,5 months: 22,9 months in tiragolumab + atezolizumab arm versus 16,7 months in placebo + atezolizumab arm, HR: 0,81 (95% CI: 0,63, 1,03)].[20] No new safety signals were identified and the trial remains blinded to investigators and patients.[21]
Tiragolumab also shows encouraging efficacy in hepatocellular carcinoma setting. In the MORPHEUS-liver trial, tiragolumab + atezolizumab + bevacizumab significantly improved response rate and PFS in both patients with positive PD-L1 expression and with negative PD-L1 expression.[22]
In small-cell lung cancer, tiragolumab didn't show any OS and PFS benefit in the SKYSCRAPER-02 trial,[23] but its development in SCLC setting is being continued as consolidation therapy for patients with limited-stage SCLC who have not progressed during/after chemotherapy and radiotherapy (NCT04308785).
In the Skyscraper-04 trial assessing the efficacy and safety of tiragolumab in patients who have recurrent, PD-L1 positive cervical cancer, the combination of tiragolumab and atezolizumab, although improved response rate in both PD-L1 low and PD-L1 high subgroups, only did so marginally and non-significantly.[24]
The combination of tiragolumab, atezolizumab, and platinum-containing chemotherapy improved PFS and OS compared with comparator arms in esophageal cancer patients in the phase II MORPHEUS-EC trial and the phase III SKYSCRAPER-08 trial.[25][26]
See also
References
Further reading
- Riquelme P, Haarer J, Kammler A, Walter L, Tomiuk S, Ahrens N, Wege AK, Goecze I, Zecher D, Banas B, Spang R, Fändrich F, Lutz MB, Sawitzki B, Schlitt HJ, Ochando J, Geissler EK, Hutchinson JA (2018). "TIGIT+ iTregs elicited by human regulatory macrophages control T cell immunity". Nature Communications. 9 (2858): 2858. Bibcode:2018NatCo...9.2858R. doi:10.1038/s41467-018-05167-8. PMC 6054648. PMID 30030423.