Influenza A virus subtype H5N1 (A/H5N1) is a subtype of the influenza A virus, which causes influenza (flu), predominantly in birds. It is enzootic (maintained in the population) in many bird populations, and also panzootic (affecting animals of many species over a wide area).[1] A/H5N1 virus can also infect mammals (including humans) that have been exposed to infected birds; in these cases, symptoms are frequently severe or fatal.[2]
| Influenza A virus subtype H5N1 | |
|---|---|
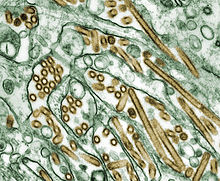 | |
| Colorized transmission electron micrograph of Avian influenza A H5N1 viruses (seen in gold) grown in MDCK cells (seen in green). | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Insthoviricetes |
| Order: | Articulavirales |
| Family: | Orthomyxoviridae |
| Genus: | Alphainfluenzavirus |
| Species: | |
| Serotype: | Influenza A virus subtype H5N1 |
| Notable strains | |
A/H5N1 virus is shed in the saliva, mucous, and feces of infected birds; other infected animals may shed bird flu viruses in respiratory secretions and other body fluids (such as milk).[3] The virus can spread rapidly through poultry flocks and among wild birds.[3] An estimated half a billion farmed birds have been slaughtered in efforts to contain the virus.[2]
Symptoms of A/H5N1 influenza vary according to both the strain of virus underlying the infection and on the species of bird or mammal affected.[4][5] Classification as either Low Pathogenic Avian Influenza (LPAI) or High Pathogenic Avian Influenza (HPAI) is based on the severity of symptoms in domestic chickens and does not predict the severity of symptoms in other species.[6] Chickens infected with LPAI A/H5N1 virus display mild symptoms or are asymptomatic, whereas HPAI A/H5N1 causes serious breathing difficulties, a significant drop in egg production, and sudden death.[7]
In mammals, including humans, A/H5N1 influenza (whether LPAI or HPAI) is rare. Symptoms of infection vary from mild to severe, including fever, diarrhoea, and cough.[5] Human infections with A/H5N1 virus have been reported in 23 countries since 1997, resulting in severe pneumonia and death in about 50% of cases.[8] As of May 2024, 889 human cases had been identified worldwide, with 463 fatalities, giving a case fatality rate of around 50%;[9] however, it is likely that this may be an overestimate given that mild infections can go undetected and under-reported.[10]
A/H5N1 influenza virus was first identified in farmed birds in southern China in 1996.[11] Between 1996 and 2018, A/H5N1 coexisted in bird populations with other subtypes of the virus, but since then, the highly pathogenic subtype HPAI A(H5N1) has become the dominant strain in bird populations worldwide.[12] Some strains of A/H5N1 which are highly pathogenic to chickens have adapted to cause mild symptoms in ducks and geese,[13][6] and are able to spread rapidly through bird migration.[14] Mammal species that have been recorded with H5N1 infection include cows, seals, goats, and skunks.[15]
Due to the high lethality and virulence of HPAI A(H5N1), its worldwide presence, its increasingly diverse host reservoir, and its significant ongoing mutations, the H5N1 virus is regarded as the world's largest pandemic threat.[16] Domestic poultry may potentially be protected from specific strains of the virus by vaccination.[17] In the event of a serious outbreak of H5N1 flu among humans, health agencies have prepared "candidate" vaccines that may be used to prevent infection and control the outbreak; however, it could take several months to ramp up mass production.[3][18][19]
Signs and symptoms
Some species of wild aquatic birds act as natural asymptomatic carriers of a large variety of influenza A viruses.[20] Symptoms of avian influenza vary according to both the strain of virus underlying the infection, and on the species of bird affected. Symptoms of influenza in wild birds may include swollen head, watery eyes, unresponsiveness, lack of coordination, respiratory distress such as sneezing or gurgling.[21]
Because of the impact of avian influenza on economically important chicken farms, avian virus strains are classified as either highly pathogenic (and therefore potentially requiring vigorous control measures) or low pathogenic. The test for this is based solely on the effect on chickens - a virus strain is highly pathogenic avian influenza (HPAI) if 75% or more of chickens die after being deliberately infected with it, or if it is genetically similar to such a strain. The alternative classification is low pathogenic avian influenza (LPAI).[22] Classification of a virus strain as either LPAI or HPAI is based on the severity of symptoms in domestic chickens and does not predict severity of symptoms in other species. Chickens infected with LPAI display mild symptoms or are asymptomatic, whereas HPAI causes serious breathing difficulties, significant drop in egg production, and sudden death.[23]Humans
Avian flu viruses, both HPAI and LPAI, can infect humans who are in close, unprotected contact with infected poultry. Incidents of cross-species transmission are rare, with symptoms ranging in severity from no symptoms or mild illness, to severe disease that resulted in death.[24][25] As of February, 2024 there have been very few instances of human-to-human transmission, and each outbreak has been limited to a few people.[26] All subtypes of avian Influenza A have potential to cross the species barrier, with H5N1 and H7N9 considered the biggest threats.[27][28]
In order to avoid infection, the general public are advised to avoid contact with sick birds or potentially contaminated material such as carcasses or feces. People working with birds, such as conservationists or poultry workers, are advised to wear appropriate personal protection equipment.[29]
The avian influenza hemagglutinin prefers to bind to alpha-2,3 sialic acid receptors, while the human influenza hemagglutinin prefers to bind to alpha-2,6 sialic acid receptors.[30][31] This means that when the H5N1 strain infects humans, it will replicate in the lower respiratory tract (where alpha-2,3 sialic acid receptors are more plentiful in humans) and consequently cause viral pneumonia.[32][33]
Between 2003 and March 2024, the World Health Organization has recorded 888 cases of confirmed H5N1 influenza, leading to 463 deaths.[34] This yields a CFR estimate of 52%. The true fatality rate may be lower because some cases with mild symptoms may not have been identified as H5N1.[35]
Virology
Influenza virus nomenclature

To unambiguously describe a specific isolate of virus, researchers use the internationally accepted Influenza virus nomenclature,[36] which describes, among other things, the species of animal from which the virus was isolated, and the place and year of collection. For example, A/chicken/Nakorn-Patom/Thailand/CU-K2/04(H5N1):
- A stands for the genus of influenza (A, B or C).
- chicken is the animal species the isolate was found in (note: human isolates lack this component term and are thus identified as human isolates by default)
- Nakorn-Patom/Thailand is the place this specific virus was isolated
- CU-K2 is the laboratory reference number that identifies it from other influenza viruses isolated at the same place and year
- 04 represents the year of isolation 2004
- H5 stands for the fifth of several known types of the protein hemagglutinin.
- N1 stands for the first of several known types of the protein neuraminidase.
Other examples include: A/duck/Hong Kong/308/78(H5N3), and A/shoveler/Egypt/03(H5N2).[37]
Genetic structure

H5N1 is a subtype of Influenza A virus, like all subtypes it is an enveloped negative-sense RNA virus, with a segmented genome.[38] Subtypes of IAV are defined by the combination of the antigenic hemagglutinin and neuraminidase proteins in the viral envelope. "H5N1" designates an IAV subtype that has a type 5 hemagglutinin (H) protein and a type-1 neuraminidase (N) protein.[39] Further variations exist within the subtypes and can lead to very significant differences in the virus's ability to infect and cause disease, as well as to the severity of symptoms.[40][41]
Influenza viruses have a relatively high mutation rate that is characteristic of RNA viruses.[42] The segmentation of its genome facilitates genetic recombination by segment reassortment in hosts infected with two different strains of influenza viruses at the same time.[43][44] Through a combination of mutation and genetic reassortment the virus can evolve to acquire new characteristics, enabling it to evade host immunity and occasionally to jump from one species of host to another.[45][46]
Prevention
Vaccine
There are several H5N1 vaccines for several of the avian H5N1 varieties, but the continual mutation of H5N1 renders them of limited use to date: while vaccines can sometimes provide cross-protection against related flu strains, the best protection would be from a vaccine specifically produced for any future pandemic flu virus strain. Daniel R. Lucey, co-director of the Biohazardous Threats and Emerging Diseases graduate program at Georgetown University has made this point, "There is no H5N1 pandemic so there can be no pandemic vaccine".[47] However, "pre-pandemic vaccines" have been created; are being refined and tested; and do have some promise both in furthering research and preparedness for the next pandemic.[48][49][50] Vaccine manufacturing companies are being encouraged to increase capacity so that if a pandemic vaccine is needed, facilities will be available for rapid production of large amounts of a vaccine specific to a new pandemic strain.
Public health
"The United States is collaborating closely with eight international organizations, including the World Health Organization (WHO), the Food and Agriculture Organization of the United Nations (FAO), the World Organization for Animal Health (OIE), and 88 foreign governments to address the situation through planning, greater monitoring, and full transparency in reporting and investigating avian influenza occurrences. The United States and these international partners have led global efforts to encourage countries to heighten surveillance for outbreaks in poultry and significant numbers of deaths in migratory birds and to rapidly introduce containment measures. The U.S. Agency for International Development (USAID) and the U.S. Department of State, the U.S. Department of Health and Human Services (HHS), and Agriculture (USDA) are coordinating future international response measures on behalf of the White House with departments and agencies across the federal government".[51]
Together steps are being taken to "minimize the risk of further spread in animal populations", "reduce the risk of human infections", and "further support pandemic planning and preparedness".[51]
Ongoing detailed mutually coordinated onsite surveillance and analysis of human and animal H5N1 avian flu outbreaks are being conducted and reported by the USGS National Wildlife Health Center, the Centers for Disease Control and Prevention, the World Health Organization, the European Commission, and others.[52]
Treatment
There is no highly effective treatment for H5N1 flu, but oseltamivir (commercially marketed by Roche as Tamiflu) can sometimes inhibit the influenza virus from spreading inside the user's body. This drug has become a focus for some governments and organizations trying to prepare for a possible H5N1 pandemic.[53] On April 20, 2006, Roche AG announced that a stockpile of three million treatment courses of Tamiflu are waiting at the disposal of the World Health Organization to be used in case of a flu pandemic; separately Roche donated two million courses to the WHO for use in developing nations that may be affected by such a pandemic but lack the ability to purchase large quantities of the drug.[54]
However, WHO expert Hassan al-Bushra has said:[55]
Even now, we remain unsure about Tamiflu's real effectiveness. As for a vaccine, work cannot start on it until the emergence of a new virus, and we predict it would take six to nine months to develop it. For the moment, we cannot by any means count on a potential vaccine to prevent the spread of a contagious influenza virus, whose various precedents in the past 90 years have been highly pathogenic.
Animal and lab studies suggest that Relenza (zanamivir), which is in the same class of drugs as Tamiflu, may also be effective against H5N1. In a study performed on mice in 2000, "zanamivir was shown to be efficacious in treating avian influenza viruses H9N2, H6N1, and H5N1 transmissible to mammals".[56] In addition, mice studies suggest the combination of zanamivir, celecoxib and mesalazine looks promising producing a 50% survival rate compared to no survival in the placebo arm.[57] While no one knows if zanamivir will be useful or not on a yet to exist pandemic strain of H5N1, it might be useful to stockpile zanamivir as well as oseltamivir in the event of an H5N1 influenza pandemic. Neither oseltamivir nor zanamivir can be manufactured in quantities that would be meaningful once efficient human transmission starts.[58] In September, 2006, a WHO scientist announced that studies had confirmed cases of H5N1 strains resistant to Tamiflu and Amantadine.[59] Tamiflu-resistant strains have also appeared in the EU, which remain sensitive to Relenza.[60][61]
Epidemiology
History
Influenza A/H5N1 was first detected in 1959 after an outbreak of highly pathogenic avian influenza in Scotland, which infected two flocks of chickens.[62] [63]The next detection, and the earliest infection of humans by H5N1, was an epizootic (an epidemic in nonhumans) of H5N1 influenza in Hong Kong's poultry population in 1997. This outbreak was stopped by the killing of the entire domestic poultry population within the territory. Human infection was confirmed in 18 individuals who had been in close contact with poultry, 6 of whom died.[64][65]
Since then, avian A/H5N1 bird flu has become widespread in wild birds worldwide, with numerous outbreaks among both domestic and wild birds. An estimated half a billion farmed birds have been slaughtered in efforts to contain the virus.[66][67]
Contagiousness

H5N1 is easily transmissible between birds, facilitating a potential global spread of H5N1. While H5N1 undergoes mutation and reassortment, creating variations which can infect species not previously known to carry the virus, not all of these variant forms can infect humans. H5N1 as an avian virus preferentially binds to a type of galactose receptors that populate the avian respiratory tract from the nose to the lungs and are virtually absent in humans, occurring only in and around the alveoli, structures deep in the lungs where oxygen is passed to the blood. Therefore, the virus is not easily expelled by coughing and sneezing, the usual route of transmission.[31][32][68]
H5N1 is mainly spread by domestic poultry, both through the movements of infected birds and poultry products and through the use of infected poultry manure as fertilizer or feed. Humans with H5N1 have typically caught it from chickens, which were in turn infected by other poultry or waterfowl. Migrating waterfowl (wild ducks, geese and swans) carry H5N1, often without becoming sick.[69][70] Many species of birds and mammals can be infected with HPAI A(H5N1), but the role of animals other than poultry and waterfowl as disease-spreading hosts is unknown.[71]
According to a report by the World Health Organization, H5N1 may be spread indirectly. The report stated the virus may sometimes stick to surfaces or get kicked up in fertilizer dust to infect people.[72]
Virulence
H5N1 has mutated into a variety of strains with differing pathogenic profiles, some pathogenic to one species but not others, some pathogenic to multiple species. Each specific known genetic variation is traceable to a virus isolate of a specific case of infection. Through antigenic drift, H5N1 has mutated into dozens of highly pathogenic varieties divided into genetic clades which are known from specific isolates, but all belong to genotype Z of avian influenza virus H5N1, now the dominant genotype.[44][43] H5N1 isolates found in Hong Kong in 1997 and 2001 were not consistently transmitted efficiently among birds and did not cause significant disease in these animals. In 2002, new isolates of H5N1 were appearing within the bird population of Hong Kong. These new isolates caused acute disease, including severe neurological dysfunction and death in ducks. This was the first reported case of lethal influenza virus infection in wild aquatic birds since 1961.[73]
Genotype Z emerged in 2002 through reassortment from earlier highly pathogenic genotypes of H5N1[74] that first infected birds in China in 1996, and first infected humans in Hong Kong in 1997.[43][44][75] Genotype Z is endemic in birds in Southeast Asia, has created at least two clades that can infect humans, and is spreading across the globe in bird populations. Mutations occurring within this genotype are increasing their pathogenicity.[76] Birds are also able to shed the virus for longer periods of time before their death, increasing the transmissibility of the virus.
Pandemic potential
Influenza viruses have a relatively high mutation rate that is characteristic of RNA viruses.[77] The segmentation of the influenza A virus genome facilitates genetic recombination by segment reassortment in hosts who become infected with two different strains of influenza viruses at the same time.[78][79] With reassortment between strains, an avian strain which does not affect humans may acquire characteristics from a different strain which enable it to infect and pass between humans - a zoonotic event.[80]
As of June 2024, there is concern about two subtypes of avian influenza which are circulating in wild bird populations worldwide, A/H5N1 and A/H7N9. Both of these have potential to devastate poultry stocks, and both have jumped to humans with relatively high case fatality rates.[81] A/H5N1 in particular has infected a wide range of mammals and may be adapting to mammalian hosts.[82]
Surveillance
The Global Influenza Surveillance and Response System (GISRS) is a global network of laboratories that monitor the spread of influenza with the aim to provide the World Health Organization with influenza control information and to inform vaccine development.[83] Several millions of specimens are tested by the GISRS network annually through a network of laboratories in 127 countries. GISRS monitors avian, swine, and other potentially zoonotic influenza viruses as well as human viruses.[84]
Transmission and host range
Infected birds transmit H5N1 through their saliva, nasal secretions, feces and blood. Other animals may become infected with the virus through direct contact with these bodily fluids or through contact with surfaces contaminated with them. H5N1 remains infectious after over 30 days at 0 °C (32 °F) (over one month at freezing temperature) or 6 days at 37 °C (99 °F) (one week at human body temperature); at ordinary temperatures it lasts in the environment for weeks. In Arctic temperatures, it does not degrade at all.[citation needed]
Because migratory birds are among the carriers of the highly pathogenic H5N1 virus, it is spreading to all parts of the world. H5N1 is different from all previously known highly pathogenic avian flu viruses in its ability to be spread by animals other than poultry.
In October 2004, researchers discovered H5N1 is far more dangerous than was previously believed. Waterfowl were revealed to be directly spreading this highly pathogenic strain to chickens, crows, pigeons, and other birds, and the virus was increasing its ability to infect mammals, as well. From this point on, avian flu experts increasingly referred to containment as a strategy that can delay, but not ultimately prevent, a future avian flu pandemic.[citation needed]
"Since 1997, studies of influenza A (H5N1) indicate that these viruses continue to evolve, with changes in antigenicity and internal gene constellations; an expanded host range in avian species and the ability to infect felids; enhanced pathogenicity in experimentally infected mice and ferrets, in which they cause systemic infections; and increased environmental stability."[85]
The New York Times, in an article on transmission of H5N1 through smuggled birds, reports Wade Hagemeijer of Wetlands International stating, "We believe it is spread by both bird migration and trade, but that trade, particularly illegal trade, is more important".[86]
On September 29, 2007, researchers reported the H5N1 bird flu virus can also pass through a pregnant woman's placenta to infect the fetus. They also found evidence of what doctors had long suspected—the virus not only affects the lungs, but also passes throughout the body into the gastrointestinal tract, the brain, liver, and blood cells.[87]
In May 2013, North Korea confirmed a H5N1 bird flu outbreak that forced authorities to kill over 160,000 ducks in Pyongyang.[88]
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | Total | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR | cases | deaths | CFR |
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8 | 5 | 62.5% | 8 | 5 | 62.5% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 2 | 0 | 0% | 3 | 0 | 0% | 1 | 1 | 100% | 1 | 0 | 0% | 8 | 1 | 12.5% | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 | 4 | 100% | 2 | 2 | 100% | 1 | 1 | 100% | 1 | 0 | 0% | 1 | 0 | 0% | 1 | 1 | 100% | 8 | 8 | 100% | 3 | 3 | 100% | 26 | 14 | 53.8% | 9 | 4 | 44.4% | 6 | 4 | 66.7% | 5 | 1 | 20.0% | 67 | 42 | 62.7% | ||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1[89] | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 8 | 5 | 62.5% | 13 | 8 | 61.5% | 5 | 3 | 60.0% | 4 | 4 | 100% | 7 | 4 | 57.1% | 2 | 1 | 50.0% | 1 | 1 | 100% | 2 | 1 | 50.0% | 2 | 2 | 100% | 2 | 0 | 0% | 6 | 1 | 16.7% | 1 | 1 | 100% | 1 | 0 | 0% | 55 | 32 | 58.2% | ||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18 | 10 | 55.6% | 25 | 9 | 36.0% | 8 | 4 | 50.0% | 39 | 4 | 10.3% | 29 | 13 | 44.8% | 39 | 15 | 38.5% | 11 | 5 | 45.5% | 4 | 3 | 75.0% | 37 | 14 | 37.8% | 136 | 39 | 28.7% | 10 | 3 | 30.0% | 3 | 1 | 33.3% | 359 | 120 | 33.4% | ||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20 | 13 | 65.0% | 55 | 45 | 81.8% | 42 | 37 | 88.1% | 24 | 20 | 83.3% | 21 | 19 | 90.5% | 9 | 7 | 77.8% | 12 | 10 | 83.3% | 9 | 9 | 100% | 3 | 3 | 100% | 2 | 2 | 100% | 2 | 2 | 100% | 1 | 1 | 100% | 200 | 168 | 84.0% | ||||||||||||||||||||||||||||||
| 3 | 2 | 66.6% | 3 | 2 | 66.6% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 | 2 | 100% | 1 | 0 | 0% | 3 | 2 | 66.7% | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 | 1 | 33.3% | 3 | 1 | 33.3% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 | 0 | 0% | 2 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17 | 12 | 70.6% | 5 | 2 | 40.0% | 3 | 3 | 100% | 25 | 17 | 68.0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12 | 4 | 33.3% | 12 | 4 | 33.3% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 4 | 0 | 0% | 5 | 0 | 0% | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 3 | 0 | 0% | 4 | 0 | 0% | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 | 3 | 100% | 29 | 20 | 69.0% | 61 | 19 | 31.1% | 8 | 5 | 62.5% | 6 | 5 | 83.3% | 5 | 5 | 100% | 7 | 2 | 28.6% | 4 | 2 | 50.0% | 2 | 1 | 50.0% | 2 | 2 | 100% | 1 | 0 | 0% | 1 | 1 | 100% | 129 | 65 | 50.0% | ||||||||||||||||||||||||||||||
| 4 | 4 | 100% | 46 | 32 | 69.6% | 98 | 43 | 43.9% | 115 | 79 | 68.7% | 88 | 59 | 67.0% | 44 | 33 | 75.0% | 73 | 32 | 43.8% | 48 | 24 | 50.0% | 62 | 34 | 54.8% | 32 | 20 | 62.5% | 39 | 25 | 64.1% | 52 | 22 | 42.3% | 145 | 42 | 29.0% | 10 | 3 | 30.0% | 4 | 2 | 50.0% | 0 | 0 | 0% | 1 | 1 | 100% | 1 | 0 | 0% | 2 | 1 | 50.0% | 6 | 1 | 16.7% | 12 | 4 | 33.3% | 10 | 2 | 20.0% | 892 | 463 | 51.9% |
2020–2024 global H5N1 outbreak
Europe
A major outbreak of a new strain of H5N1 in wild birds and poultry appeared in Russia in August 2020 and quickly spread to other parts of Europe by October.[90]
Over the winter of 2021 and 2022, avian flu spread among the population of barnacle geese on the Solway Firth, UK, with estimates of up to a third of the Svalbard population being lost;[91][92] pink-footed geese were also affected there and it seems carried the virus to new sites in northern Scotland. The disease was confirmed in sandwich terns in South Africa in April 2022.[93] In late spring 2022 avian flu outbreaks affected many species of wild bird in the United Kingdom, with heavy losses reported among seabirds returning to breed at colonies in the Northern Isles and Outer Hebrides,[94] including great skuas (bonxie) for which outbreaks had initially been reported in 2021[95] (Scotland hosts c. 60% of the world's breeding population) – the 2022 census on St Kilda showed a 64% decline on 2019 with 106 dead birds recorded so far (to 6 June),[96] gannets (1000+ birds reported dead at the Shetlands' Hermaness colony alone,[94] where there are around 26,000 breeding pairs), with many more gannets being reported dead at other colonies (Troup Head, Bass Rock, and St Kilda);[97] the range of species also seems to be expanding, with reports for many species of wildfowl, seabirds (auks, terns and gulls) and scavenging species (corvids and raptors).[98][99]
Elsewhere in Europe the virus killed hundreds (574+) of Dalmatian pelicans in Greece,[100][101] and in Israel around 6000 common cranes were found dead at Hula in December 2021.[102] A report by Scientific Task Force on Avian Influenza and Wild Birds on: "H5N1 Highly Pathogenic Avian Influenza in poultry and wild birds: Winter of 2021/2022 with focus on mass mortality of wild birds in UK and Israel" summarises the situation up to 24 January 2022 and mentions that "H5N8 HPAI is still responsible for poultry and wild bird cases mainly in Asia, H5N1 has now in effect replaced this subtype in Africa and Eurasia in both poultry and wild birds".[103]
The 2022–2023 season was also the worst recorded outbreak in the United Kingdom, with the British government requiring a so-called "poultry lockdown" which required that farmers keep their birds indoors.[104] Meanwhile, an outbreak of H5N1 on a Spanish mink farm led researchers to believe that they had observed the first case of mammal-to-mammal transmission of H5N1.[105] Human cases were reported in Spain in November 2022, and in the UK in May 2023.[90]
Asia
By November 2020, large outbreaks of the new strain of H5N1 had started to spread into wild birds and farmed poultry across Asia. In February 2023, human cases were reported in Cambodia.[90]
Africa
Large losses of poultry and wild birds to H5N1 started to occur in Africa in November 2021 and continued through 2022.[90]
Americas
Similar to 2021 reports, outbreaks were noted from gannet colonies in Canada, with thousands of birds dead in June 2022,[106] as well as common eiders and great black-backed gulls.[107] Prior to that there were reports of spread in wild birds in over 30 states in the US, including major mortalities in a double-crested cormorant colony in Barrington, Illinois,[108][109] the virus also spreading to scavengers including three bald eagles in Georgia.[110] Mass die-offs of both birds and mammals were noted in Peru during the 2022–2023 season.[111] In particular, the Peruvian government reported the deaths of approximately 63,000 birds as well as 716 sea lions, with the WHO noting that mammalian spillovers needed to be "monitored closely".[104][112] In the United States, the 2022–2023 avian outbreak was the worst since H5N1 was first detected.[104]
Ecuador entered into a three-month "animal-health emergency" on 29 November 2022, just days after its first case was reported, whereas Argentina and Uruguay both declared "national sanitary emergencies" on 15 February 2023, after their respective first cases were discovered.[113] On 22 May 2023, Brazil, as the world's largest exporter of chicken meat, declared a 180-day emergency following several cases detected in wild birds and created an emergency operations center to plan for and mitigate potential further spread of H5N1.[114] Human cases were reported in Ecuador and Chile.[90]
In March 2024, H5N1 infections were recorded for the first time in deceased and sick livestock located in the United States. Goats and cows in three states became ill after exposure to wild birds and culled poultry.[115] In early April, H5N1 was reported to have spread amongst dairy cow herds in multiple states of the USA, indicating cow-to-cow spread, possibly occurring while the animals were being milked.[116] A dairy worker in Texas also became infected, with conjunctivitis being the main symptom.[117]
On 22 May 2024, a farm worker in Michigan was infected with the H5N1 virus due to their regular exposure to infected dairy cows. The person had mild symptoms and recovered.[118] On 30 May, it was announced that a second Michigan farm worker from a different dairy farm had been diagnosed with H5N1 after exhibiting respiratory symptoms.[119][120] As of July 3, five American cases were reported.[121]
Antarctica
H5N1 was detected in dead birds on the Antarctic mainland for the first time in February 2024.[122]
Arctic
In December 2023, conservation officials confirmed that a polar bear had died of H5N1 near Alaska's northernmost city, Utqiagvik.[123]
Australia
In May 2024, H5N1 was detected for the first time in Australia after a human child who had returned to the country from India tested positive. The child had a severe infection but recovered.[124]
Mammalian infections
H5N1 transmission studies in ferrets (2011)
Novel, contagious strains of H5N1 were created by Ron Fouchier of the Erasmus Medical Center in Rotterdam, the Netherlands, who first presented his work to the public at an influenza conference in Malta in September 2011. Three mutations were introduced into the H5N1 virus genome, and the virus was then passed from the noses of infected ferrets to the noses of uninfected ones, which was repeated 10 times.[125] After these 10 passages the H5N1 virus had acquired the ability of transmission between ferrets via aerosols or respiratory droplets.
After Fouchier offered an article describing this work to the leading academic journal Science, the US National Science Advisory Board for Biosecurity (NSABB) recommended against publication of the full details of the study, and the one submitted to Nature by Yoshihiro Kawaoka of the University of Wisconsin describing related work. However, after additional consultations at the World Health Organization and by the NSABB, the NSABB reversed its position and recommended publication of revised versions of the two papers.[126] However, then the Dutch government declared that this type of manuscripts required Fouchier to apply for an export permit in the light of EU directive 428/2009 on dual use goods.[note 1] After much controversy surrounding the publishing of his research, Fouchier complied (under formal protest) with Dutch government demands to obtain a special permit[127] for submitting his manuscript, and his research appeared in a special issue of the journal Science devoted to H5N1.[128][129][130] The papers by Fouchier and Kawaoka conclude that it is entirely possible that a natural chain of mutations could lead to an H5N1 virus acquiring the capability of airborne transmission between mammals, and that a H5N1 influenza pandemic would not be impossible.[131]
In May 2013, it was reported that scientists at the Harbin Veterinary Research Institute in Harbin, China, had created H5N1 strains which passed between guinea pigs.[132]
In response to Fouchier and Kawaoka's work, a number of scientists expressed concerns with the risks of creating novel potential pandemic pathogens, culminating in the formation of the Cambridge Working Group, a consensus statement calling for an assessment of the risks and benefits of such research.[133][134]
Mammal-to-mammal transmission (2022–2024)
Although mammals, including humans, had become infected with H5N1 bird flu strains in the past, these cases had ostensibly been caused by direct exposure to infected birds, such as through consumption of birds by wildlife or exposure to infected poultry by farmers. In contrast, the October 2022 mammalian outbreak of H5N1 on a Spanish mink farm showed evidence of being the first recorded case of mammal-to-mammal transmission, with 4 percent of the farm's mink population dying from H5N1-related haemorrhagic pneumonia.[105][135] The mink respiratory tract is particularly well suited to act as a pathway of viral transmission into humans, which has concerned public health professionals due to the production of all but one approved human vaccine requiring the eggs of chickens, which H5N1 kills at a 90–100 percent fatality rate.[136] Infected mink in Spain were also found to have exhibited the "PB2" viral mutation found when H5N1 jumped into pigs over a decade prior, adding to fears that farms could be acting as incubators and/or reservoirs of the virus, similar to the role of minks in SARS-CoV-2.[105]
As of January 2023, fifteen species of wild and captive mammals had become infected with H5N1 throughout the United States.[137] A mass Caspian seal die-off in December 2022, with 700 infected seals found dead along the Caspian Sea coastline of Russia's Dagestan republic, worried researchers regarding the possibility that wild mammal-to-mammal spread had begun.[138] A similar mass die-off of 95% of southern elephant seal pups in 2023 also raised concerns of mammal-to-mammal spread, as nursing pups would have had less exposure to birds.[139]
In April 2024, spread of H5N1 amongst dairy cow herds in nine states of the USA strongly indicated the presence of cow-to-cow transmission possibly occurring while the animals were being milked.[116][140] Although mortality in bovines infected with H5N1 is rare, abundant virus shedding in the milk is evident.[116] Around 50% of cats that lived on the affected dairy farms and were fed unpasteurised milk from symptomatic cows died within a few days from severe systemic influenza infection, raising significant concerns of cross-species mammal-to-mammal transmission.[141]
Society and culture
H5N1 has had a significant effect on human society, especially the financial, political, social, and personal responses to both actual and predicted deaths in birds, humans, and other animals. Billions of dollars are being raised and spent to research H5N1 and prepare for a potential avian influenza pandemic. Over $10 billion have been spent and over 200 million birds have been killed to try to contain H5N1.[142][143][144][145][146][147][148][149][150]
People have reacted by buying less chicken, causing poultry sales and prices to fall.[151] Many individuals have stockpiled supplies for a possible flu pandemic. International health officials and other experts have pointed out that many unknown questions still hover around the disease.[152]
Dr. David Nabarro, Chief Avian Flu Coordinator for the United Nations, and former Chief of Crisis Response for the World Health Organization has described himself as "quite scared" about H5N1's potential impact on humans. Nabarro has been accused of being alarmist before, and on his first day in his role for the United Nations, he proclaimed the avian flu could kill 150 million people. In an interview with the International Herald Tribune, Nabarro compares avian flu to AIDS in Africa, warning that underestimations led to inappropriate focus for research and intervention.[153]
See also
Notes
References
Citations
Sources
- Analysis of the efficacy of an adjuvant-based inactivated pandemic H5N1 influenza virus vaccine. https://link.springer.com/article/10.1007%2Fs00705-019-04147-7 Ainur NurpeisovaEmail authorMarkhabat KassenovNurkuisa RametovKaissar TabynovGourapura J. RenukaradhyaYevgeniy VolginAltynay SagymbayAmanzhol MakbuzAbylay SansyzbayBerik Khairullin
Research Institute for Biological Safety Problems (RIBSP), Zhambyl Region, Republic of Kazakhstan
External links


- Influenza Research Database – Database of influenza genomic sequences and related information.
- WHO World Health Organization
- WHO's Avian Flu Facts Sheet for 2006
- Epidemic and Pandemic Alert and Response Guide to WHO's H5N1 pages
- Avian Influenza Resources (updated) – tracks human cases and deaths
- National Influenza Pandemic Plans
- WHO Collaborating Centres and Reference Laboratories Centers, names, locations, and phone numbers
- FAO Avian Influenza portal Archived 2012-01-26 at the Wayback Machine Information resources, animations, videos, photos
- FAO Food and Agriculture Organisation – Bi-weekly Avian Influenza Maps – tracks animal cases and deaths
- FAO Bird Flu disease card
- FAO Socio-Economic impact of AI Projects, Information resources
- OIE World Organisation for Animal Health – tracks animal cases and deaths
- Official outbreak reports by country Archived 2012-12-13 at the Wayback Machine
- Official outbreak reports by week
- Chart of outbreaks by country Archived 2012-04-19 at the Wayback Machine
- Health-EU Portal EU response to Avian Influenza.
- Avian influenza – Q & A's factsheet from European Centre for Disease Prevention and Control
- United Kingdom
- Exotic Animal Disease Generic Contingency Plan – DEFRA generic contingency plan for controlling and eradicating an outbreak of an exotic animal disease. PDF hosted by BBC.
- UK Influenza Pandemic Contingency Plan by the National Health Service – a government entity. PDF hosted by BBC
- UK Department of Health Archived 2009-07-09 at the Wayback Machine
- United States
- Center for Infectious Disease Research and Policy Archived 2013-06-17 at the Wayback Machine Avian Influenza (Bird Flu): Implications for Human Disease – An overview of Avian Influenza
- PandemicFlu.Gov U.S. Government's avian flu information site
- USAID U.S. Agency for International Development – Avian Influenza Response
- CDC, Centers for Disease Control and Prevention – responsible agency for avian influenza in humans in US – Facts About Avian Influenza (Bird Flu) and Avian Influenza A (H5N1) Virus
- USGS – NWHC National Wildlife Health Center – responsible agency for avian influenza in animals in US
- Wildlife Disease Information Node A part of the National Biological Information Infrastructure and partner of the NWHC, this agency collects and distributes news and information about wildlife diseases such as avian influenza and coordinates collaborative information sharing efforts.
- HHS U.S. Department of Health & Human Services's Pandemic Influenza Plan
























